Selecting a treatment. Deciding on the right treatment for ECD involves collaboration between the patient and their doctors. Fortunately, ECD patients have treatment options, some of which have proven to be very effective for most patients. A few patients with asymptomatic disease not involving major organs may enter a watch-and-wait period with no treatment. However, treatment is generally recommended, especially for those with critical organ involvement, such as the heart, brain, or central nervous system.
Treatment vs. cure. Although there are effective treatments for ECD, a cure is yet to be found. The best treatments available today are called targeted treatments and are usually successful in controlling and often shrinking ECD lesions. At present, these treatments normally must be continued indefinitely, or the disease will most likely begin to progress again. However, with successful treatment, ECD can often be controlled as more of a chronic disease.
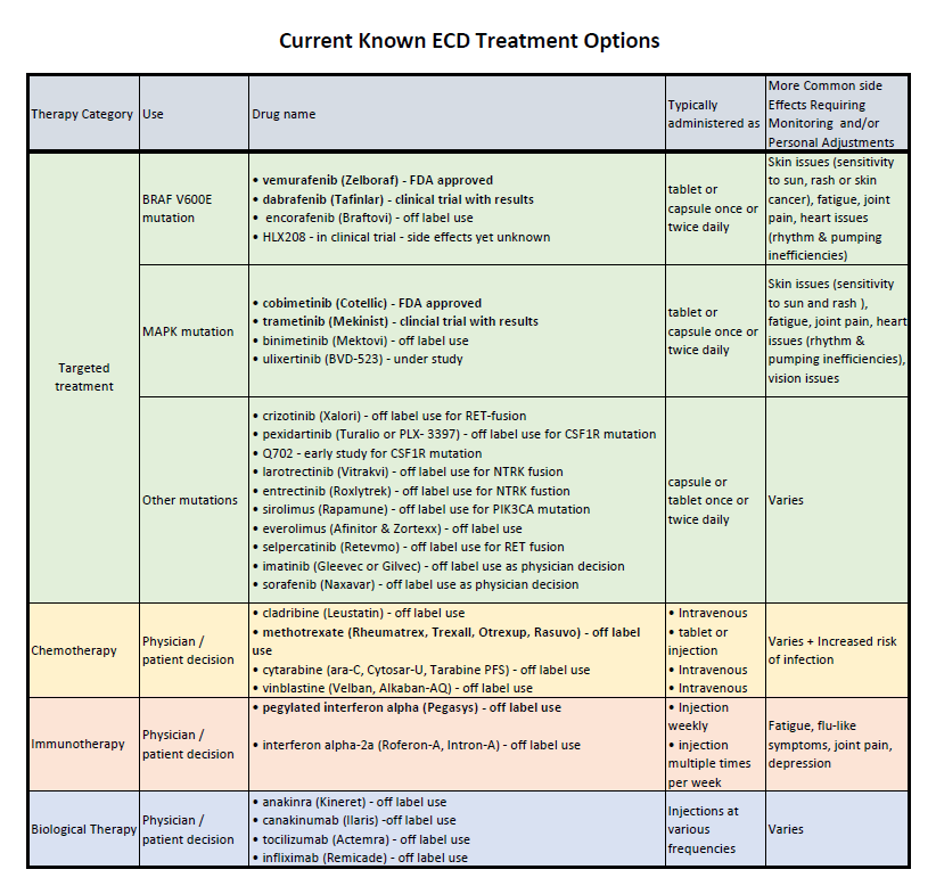
Types of Treatments. Typical ECD treatments fall into one of three categories: (1) targeted treatments, (2) chemotherapy, or (3) immunotherapy.
Targeted Therapies. These are the newest and generally most promising treatments available for ECD. They typically halt the progression of ECD in most organs, although brain involvement must be watched very carefully. For some patients, it can be difficult for targeted treatments to cross the blood/brain barrier, reducing their effectiveness in halting ECD progression in the brain. Targeted treatments are expensive and may be challenging to obtain in some parts of the world.
Targeted treatments in ECD block the action of the various MAPK pathway mutations. The choice of targeted agent is often directed by the mutations present in the ECD tissue based on genetic testing.
BRAF V600E Positive ECD. Approximately 50% of patients will test positive for the BRAF V600E mutation. Treatment options for these patients typically include a BRAF inhibitor, a MEK inhibitor, or a combination of both. Commonly used BRAF inhibitors include vemurafenib, dabrafenib, and encorafenib. Commonly used MEK inhibitors include cobimetinib, trametinib, or binimetinib. In the USA, vemurafenib and cobimetinib are FDA-approved treatments for ECD.
BRAF V600E negative, MAPK Mutated ECD. The majority of patients who test negative for the BRAF V600E mutation, will have a different mutation in what is called the MAPK pathway (also known as the Ras-Raf-MEK-ERK pathway). This pathway is a chain of proteins in the cell that communicates a signal from a receptor on the surface of the cell to the DNA in the nucleus of the cell. These signals control the cells’ proliferation, differentiation, development, inflammatory responses, and programmed cell death. Typical treatments considered for ECD patients who test negative for BRAF V600E mutations include MEK inhibitors. Commonly used MEK inhibitors include cobimetinib, trametinib or binimetinib. In the USA, cobimetinib is an FDA-approved treatment for ECD.
Non-MAPK Mutated Patients. Infrequently, ECD patients may have mutations that are not in the MAPK pathway. Currently, the following mutations have been discovered in a very small percentage of ECD patients with limited reporting of the listed corresponding treatment.
| Discovered mutation in the ECD lesion | Possible Therapy |
| ALK fusion | Crizotinib |
| CSF1R mutation | Pexidartinib |
| NTRK gene fusion | Larotrectinib |
| NTRK gene fusion | Entrectinib |
| PIK3CA mutation | Sirolimus |
| RET fusion | Selpercatinib |
Other targeted treatments. Prior to understanding the genetic mutations seen in ECD, other targeted treatments were used, but without the dramatic good results often seen in the above treatments. Some earlier targeted treatments used for ECD included imatinib (tyrosine inhibitor) and sorafenib (kinase inhibitor.)
Dosage of targeted treatments. It should be noted that most ECD patients can often only tolerate a low dosage of targeted treatment drugs. For this reason, the administered dosage prescribed for ECD patients is often lower than that used in the treatment of other diseases. Currently, although these treatments must often be continued indefinitely, further dosage reductions are often possible once a patient’s disease is fully stabilized on treatment. Patients should always discuss with their doctor any change in the dosage of their treatment prior to making any changes.
Treatment form. In most cases, all the targeted treatments are administered in pill form, taken once or twice daily.
Side Effects. Side effects of targeted treatments must be managed as a partnership between the patient and their medical team. Patients should always ask their medical team about possible side effects whenever beginning any treatment. The common side effects of BRAF inhibitors include rash, joint pains, and sun-sensitivity of skin. The common side effects of MEK inhibitors include rash, diarrhea, and swelling of legs. Rare side effects of BRAF inhibitors include skin cancers or heart rhythm problems, and of MEK inhibitors include vision disturbances and heart failure.
Treatment Cost. The cost of targeted treatment can sometimes be very high. In some countries, insurance and government payers will cover the majority of the cost of treatment. In some locations, there may be organizations that can help with the residual cost of treatment, depending on patient income. Yet, in other locations, access to targeted treatments prove to be extremely limited. Patients should speak to their medical team about the costs of these treatments and discuss payment options. The ECDGA is available to work with patients and their medical teams to help search out payment options where possible.
Chemotherapy. Chemotherapy uses drugs that destroy cancer cells or other rapidly dividing cells. Multiple chemotherapy regimens have been used in the treatment of ECD. These include: cladribine and methotrexate. Small studies have shown that some patients respond well to chemotherapy, although the response rate is lower than that of targeted treatments. An advantage of these treatments is that some patients have experienced a prolonged response with limited duration of treatment.
Cladribine. Prior to the availability of targeted treatments, cladribine was used and studied as a treatment for ECD. It showed moderate efficacy for ECD patients. Typically, patients received cladribine for 5 days, every 28 days, for 2-3 months via intravenous injections.
Methotrexate. The use of methotrexate as a treatment for ECD has shown a low response rate. However, this treatment is normally well-tolerated and thus could be beneficial to those for whom it works. Methotrexate can be administered as an infusion, injection or by tablet. For ECD patients it is normally administered as a weekly injection into the muscle.
Other chemotherapies. Other chemotherapy drugs used less often in the treatment of ECD include cytarabineand vinblastine.
Immunotherapy. Immunotherapy can work either by stimulating or suppressing the immune system to shrink ECD lesions.
Interferon. The first treatment discovered for ECD was interferon, a form of immunotherapy. Where available, pegylated interferon alpha is the preferred interferon treatment because it is administered less often. However, this formulation is not available in all countries. Interferon alpha-2a has been used in the treatment of ECD and simply needs to be taken more often. Interferon is normally administered at home via a shot under your skin or into a muscle. This treatment must most often continue indefinitely. Although some patients can easily tolerate interferon treatment, many patients report flu-like feelings when becoming acclimated to the treatment. This treatment has been found to slow the progression of ECD.
Sirolimus. Sirolimus, a form of immunosuppressive therapy, was shown in a very small study to have moderate efficacy for a small group of ECD patients. This treatment is normally administered in tablet or liquid form once a day.
Biological Therapies. Biological therapy is a type of treatment that suppresses the abnormal chemicals (cytokines) produced by the ECD cells to cause inflammation, resulting in shrinkage of lesions.
Anakinra. Small studies have shown that some patients have responded to Anakinra as a treatment option for ECD. Anakinra is normally administered as an injection under the skin. The study of anakinra as a stand-alone treatment for ECD has been limited.
Other biologic treatments. Less often used biologic treatments include canakinumab, tocilizumab, and infliximab.
Clinical Trials. Because of the rarity of this disease, clinical trials were not historically conducted to assess the effectiveness of treatments. Early documented treatments were based on case studies conducted with very small groups of patients, sometimes just a single patient. However, this is changing. Today there are several studies and clinical trials open to ECD patients in some countries. When ECD patients enroll in a clinical trial, they can have access to some of the newest and best treatments available to ECD patients. All patients are encouraged to talk with their medical team about whether a clinical trial would be appropriate for their situation. Clinical trials not only allow patients access to the newest treatment options but also pave the way for treatments to be scientifically proven effective in the treatment of ECD. This has led to the FDA-approval of two ECD treatments. FDA-approval helps all ECD patients gain access to the treatment. There is strong hope that new treatments will be found in the not-too-distant future that will be easier to tolerate.
For more information see:
- National Comprehensive Cancer Network (NCCN) Histiocytic Neoplasms, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology.
- Blood Journal article, https://ashpublications.org/blood/article/135/22/1929/452713/Erdheim-Chester-disease-consensus-recommendations
These publications have been authored by leading experts in the diagnosis and treatment of ECD. If a patient is being seen by a doctor with little ECD awareness or knowledge, it is highly suggested that these documents be shared with them.
Last updated: June 14, 2024