Diagnostic Overview
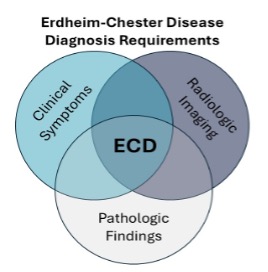
ECD is often a challenge to diagnose, given non-specific symptoms and similarities to multiple other medical conditions. The diagnosis is often delayed by years or even decades in some cases. A definitive diagnosis is usually based on a review of ECD-involved biopsy in combination with radiologic findings from PET-CT, CT, MRI, or bone scan. Mutational testing of biopsies is also becoming increasingly important in diagnosing ECD. Nearly 90 % or more of ECD patients seem to have activation in the MAPK pathway cascade caused by a genetic mutation in the MAPK pathway. These mutations are believed to be acquired during a person’s lifetime (somatic) rather than inherited; therefore, these mutations are not passed through generations. If there is a suspicion of ECD, it is important for patients to be seen at specialized centers with expertise in hematology, pathology, radiology, neurology, and other subspecialties to accurately diagnose ECD and implement treatment in a timely manner.
Imaging is used for diagnosis
Non-invasive scans such as CT scan, PET/CT scan (head to toes), MRI, bone scan, or echocardiogram are typical tests used to diagnose ECD. The PET/CT is considered the most helpful in accurately diagnosing ECD and identifying the extent of the disease.
Biopsy is used for diagnosis
If a mass or lesion is found within the body, a tissue biopsy will be performed as part of the diagnostic workup for ECD. A biopsy is often performed using a needle, but sometimes, a surgical biopsy is needed to get enough tissue and arrive at an appropriate diagnosis. A pathologist will study the tissue sample that is obtained via the biopsy. ECD-affected tissue usually contains clusters of foamy (fat-containing) histiocytes with signs of chronic inflammation, often with Touton-type giant cells and fibrosis. The pathologist will conduct additional stains (dye tests) to check if specific markers are present in the ECD histiocytes. Skin and perirenal tissues are often more informative for the diagnosis and molecular analyses.
Genetic Testing
Pathologists are increasingly performing genetic testing on a biopsy sample if ECD is suspected. If an ECD-known mutation is found, it will help lead to a more definitive diagnosis and is often needed to select the best treatment for a patient. Mutation testing does not always show a mutation, and it is important to remember that a mutation does not need to be found to achieve an ECD diagnosis or to allow for treatment.
Diagnosis
To arrive at a correct ECD diagnosis or to rule out an ECD diagnosis, doctors rely upon the findings of a biopsy of affected tissue and related imaging studies. A trained pathologist should review tissue samples, and the imaging should be reviewed by a radiologist, both of whom have knowledge of ECD. It is critical for the pathologist, radiologist, and physician seeing the patient to communicate well with each other to arrive at the diagnosis.
Systemic search for all areas of involvement
Once preliminary tests indicate an ECD diagnosis, it is important to make a systematic study of the organs possibly affected, including the skeleton, lungs, heart, large vessels, central nervous system, kidneys, eyes, pituitary, and/or skin. An individual with ECD needs to be seen by many specialists to obtain an accurate baseline to determine the extent of the disease. This helps the medical team monitor ECD to see if treatments are effective and to take quick action if the disease begins to progress after treatment begins. Tests that should be expected include:
- Blood tests.
- Scans to include PET/CT, possible bone scan, MRI (essential for the brain), ultrasound, electrocardiogram, and echocardiogram.
- Biopsy of soft tissue and/or bone.
- Specialist examinations, depending on involved sites, to include neurology (brain), cardiology (heart), nephrology (kidney), endocrinology (hormones), dermatology (skin), ophthalmology (eyes), pulmonology (lung), psychology (mental health), and perhaps others.
Checking for other related blood disorders
Some of these tests are specific checks to rule out additional blood disorders found in a small percentage of ECD patients. Studies have shown that about 10% of ECD patients have other blood cancers, including myelodysplastic syndrome (MDS), myeloproliferative neoplasm (MPN), or chronic myelomonocytic leukemia (CMML). It is important to test for these conditions so appropriate treatment and monitoring can be planned.
For More Information
The following publications have been authored by leading experts in diagnosing and treating ECD. It is highly suggested that these documents be shared with any doctor unfamiliar with ECD and seeing an individual with ECD.
- National Comprehensive Cancer Network (NCCN) Histiocytic Neoplasms, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology.
- Blood Journal article, https://ashpublications.org/blood/article/135/22/1929/452713/Erdheim-Chester-disease-consensus-recommendations
Last updated: November 15, 2024